When Nighttime Grinding Destroys Your Jaw: The Hidden Path from Bruxism to TMJ Arthritis
Story-at-a-Glance
- Nighttime bruxism causes TMJ arthritis through mechanical overload that degrades cartilage, with sustained clenching creating shear stresses exceeding the disc’s tensile strength after just 50 seconds
- The inflammatory cascade triggered by bruxism includes elevated cytokines (TNF-α, IL-1β) and matrix metalloproteinases that systematically break down joint cartilage and bone
- Meta-analysis reveals that bruxism increases TMD odds by 2.25 times, with sleep bruxism specifically elevating risk by 1.98 times
- Magnesium deficiency emerges as a key factor, with research linking low magnesium to increased muscle hyperactivity, stress sensitivity, and disrupted sleep patterns that perpetuate grinding
- Omega-3 fatty acids and curcumin demonstrate powerful anti-inflammatory properties that may protect cartilage from degradation while reducing joint pain and stiffness
- Combined supplementation with magnesium glycinate (for muscle relaxation), EPA/DHA omega-3s (minimum 1g each), and bioavailable curcumin offers a multi-pronged approach to both prevention and management
- Early intervention matters—addressing nighttime bruxism before arthritis develops can prevent irreversible cartilage damage and preserve long-term jaw function
The alarm clock reads 3:47 AM when Sarah’s husband gently shakes her awake. “You’re grinding again,” he whispers, his concern evident even through his drowsiness. Sarah touches her jaw—it’s sore, tight, somehow both numb and aching at once. By morning, she’ll have a headache that throbs at her temples, a familiar unwelcome companion that’s been showing up more frequently over the past year.
What Sarah doesn’t yet know is that her nighttime teeth grinding isn’t just causing morning discomfort. This condition affects roughly 8-10% of the population. Deep within her temporomandibular joints (TMJs), a destructive process is underway—one that could lead to permanent arthritis if left unaddressed. The connection between nighttime bruxism causing temporomandibular joint arthritis represents one of oral medicine’s most insidious yet preventable pathways to chronic pain.
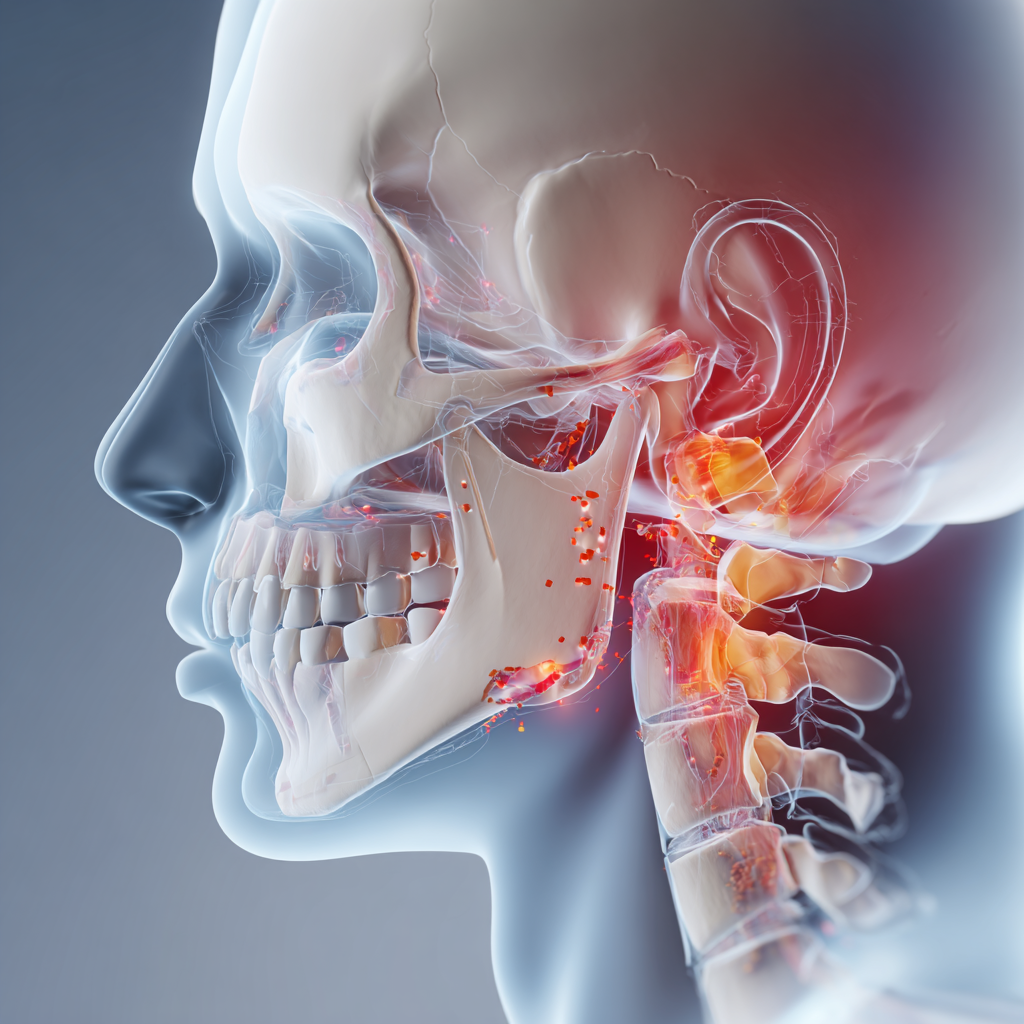
The Biomechanics of Destruction: How Grinding Becomes Arthritis
Your temporomandibular joints are engineering marvels—complex hinges connecting your jawbone to your skull. They allow you to chew, speak, yawn, and perform countless other movements we take for granted. According to Johns Hopkins Medicine, these joints consist of the mandible (lower jaw) and the temporal bone of the skull. They also include muscles, ligaments, and a fibrocartilage disc that cushions the joint during movement.
When nighttime bruxism enters the picture, this intricate system faces forces it was never designed to handle. While awake, we typically apply 20-40 pounds of force when chewing. During sleep bruxism, however, that force can skyrocket to 250 pounds—more than six times normal pressure, applied rhythmically throughout the night when our protective reflexes are offline.
Research published in the International Journal of Oral Science used finite element modeling to examine what happens inside the TMJ during bruxism episodes. The findings were striking: sustained clenching during awake bruxism produced the most detrimental activity for the TMJ disc. This created overload stresses that could lead to severe tissue damage. The researchers found that tensile stresses exceeded the disc’s ultimate strength of 2.02-2.62 MPa. This occurred after just 50 seconds of sustained clenching at 20% of maximum voluntary contraction.
But here’s what makes nighttime bruxism causing temporomandibular joint arthritis particularly insidious: the damage accumulates silently. The TMJ’s articular disc is a viscoelastic tissue. This means its response to force depends on both the magnitude and duration of loading. Cyclic loading during rhythmic grinding, combined with sustained clenching episodes, creates a perfect storm for cartilage breakdown.
The Inflammatory Cascade: From Mechanical Stress to Arthritis
When repetitive mechanical overload damages the TMJ disc and cartilage, the body doesn’t simply let it happen quietly. Instead, a complex inflammatory response kicks in—and paradoxically, this “repair” response often accelerates the degenerative process.
Research in Arthritis Research & Therapy reveals how the biochemical pathways unfold. The mechanical stress from bruxism triggers the release of pro-inflammatory cytokines. These include tumor necrosis factor-alpha (TNF-α) and interleukin-1 beta (IL-1β). These signaling molecules don’t just cause pain. They actively stimulate the production of matrix metalloproteinases (MMPs), enzymes that break down the collagen and proteoglycans forming the cartilage’s structural framework.
The cascade intensifies: MMPs degrade the extracellular matrix. Simultaneously, TNF-α and IL-1β increase RANKL secretion from osteoblasts and synovial fibroblasts. This promotes osteoclast formation and bone resorption. The NF-κB signaling pathway becomes activated, perpetuating inflammation. Osteopontin, another inflammatory agent, stimulates even more MMP production through the same pathway.
In a study on autoimmune arthritis in mice, researchers demonstrated an important finding. Elevated circulating inflammatory cytokines can create a pro-inflammatory environment within the TMJ even without direct synovial inflammation. The temporomandibular joints of arthritic mice showed aggrecanase- and MMP-mediated loss of glycosaminoglycan-containing aggrecan. This is the very substance that gives cartilage its ability to withstand compression.
What does this mean for someone with nighttime bruxism? Each grinding episode isn’t just mechanically wearing down cartilage. It’s triggering biochemical warfare against your own joint tissues.
The Evidence: Just How Strong Is the Link?
For years, the relationship between bruxism and TMJ disorders remained controversial, with some researchers questioning whether the association was truly causal. A landmark meta-analysis published in Evidence-Based Dentistry in 2023 finally provided definitive numbers.
After reviewing 1,651 studies and analyzing 20 high-quality investigations, the researchers found that bruxism increased the odds of developing TMD by 2.25 times (OR = 2.25, 95% CI 1.94-2.56). When broken down by type, sleep bruxism increased TMD odds by 1.98 times, while awake bruxism elevated risk by 2.51 times.
Additional research in the Journal of Oral Rehabilitation examined 110 participants using polysomnographic diagnosis of sleep bruxism combined with the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD). While they found no significant differences in group-III diagnoses (arthralgia, arthritis, arthrosis) between bruxers and non-bruxers in their cross-sectional analysis, they noted important predictors. Somatization and female gender were significant predictors of TMD progression—factors often associated with stress-related bruxism.
Perhaps most compelling, a study examining awake and sleep bruxism using DC/TMD criteria found that both types were associated with pain-related TMD and intra-articular joint disorders. Notably, awake bruxism was specifically associated with arthralgia—joint pain—suggesting that different bruxism patterns may lead to distinct TMJ complications.
These aren’t just abstract statistics. They represent real people like Sarah, whose nightly grinding is silently elevating her risk of developing permanent arthritis in one of the body’s most frequently used joints.
Save This Article for Later – Get the PDF Now
The Magnesium Connection: A Missing Piece of the Puzzle
Here’s something most dentists don’t tell patients about nighttime bruxism causing temporomandibular joint arthritis: nutritional deficiencies may be fueling the fire. Magnesium deficiency has emerged as a potentially significant contributor to both the initiation and perpetuation of bruxism.
A comprehensive review in Experimental and Therapeutic Medicine examined how nutrient insufficiencies contribute to bruxism pathogenesis. The evidence surrounding magnesium is particularly intriguing. This essential mineral regulates over 300 enzymatic reactions in the body. These include reactions governing muscle contraction, nerve transmission, and stress response.
When magnesium levels drop, several bruxism-promoting changes occur:
Neuromuscular excitability increases. Magnesium acts as a natural calcium blocker at neuromuscular junctions. Without adequate magnesium, calcium floods into muscle cells more easily, triggering contractions. The small muscles around the jaw become hyperactive, setting the stage for clenching and grinding.
Stress sensitivity amplifies. Magnesium deficiency reduces GABA (gamma-aminobutyric acid) production, the brain’s primary calming neurotransmitter. Simultaneously, it elevates cortisol. Research cited in the review found that experimentally-induced magnesium deficiency in animals disrupted sleep patterns and increased the amplitude of daily variation in slow-wave sleep delta power.
Sleep quality deteriorates. In humans, chronic sleep deprivation progressively decreases intracellular magnesium levels, creating a vicious cycle. Poor sleep increases bruxism, while depleted magnesium worsens sleep quality.
One study referenced in the review found that patients suffering from migraines and tension-type headaches presented with significantly lower serum and salivary magnesium levels. These symptoms are extremely common in bruxism sufferers. Hypomagnesemia makes cerebral arteries more sensitive to CO2, promoting cerebral vasospasm and headaches.
Clinical observations from dental practitioners support these mechanistic findings. One case series documented patients with bruxism who experienced symptom reduction after magnesium supplementation. Highly bioavailable forms like magnesium glycinate and citrate proved particularly effective.
The recommended approach? Sources suggest taking magnesium glycinate at doses of 200-400mg daily. This form combines high absorption with the calming effects of the amino acid glycine. Importantly, magnesium glycinate doesn’t cause the digestive disturbances associated with other forms like magnesium oxide.
But here’s a critical insight many miss: supplementing magnesium addresses only one piece of the nighttime bruxism puzzle. It may reduce the frequency and intensity of grinding by relaxing jaw muscles and improving sleep. However, it doesn’t directly address the inflammatory arthritis process once it’s begun.
Fighting Fire with Fire: Anti-Inflammatory Supplements for TMJ Protection
If magnesium helps prevent bruxism episodes, what protects the temporomandibular joint once inflammation has taken hold? This is where we must shift our focus to compounds that specifically target the inflammatory cascade driving arthritis progression.
Omega-3 Fatty Acids: The Inflammation Interrupters
The polyunsaturated omega-3 fatty acids EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) have earned significant attention in arthritis research. According to Scientific American’s review of anti-inflammatory supplements with the strongest evidence, omega-3 fatty acids rank among just three compounds with robust human trial support.
How do they work? The body metabolizes EPA and DHA into specialized signaling molecules that block the production of inflammatory cytokines and disrupt the nuclear factor κB (NF-κB) pathway. This is the same pathway driving cartilage breakdown in TMJ arthritis. Multiple studies suggest omega-3 supplements can reduce markers of chronic inflammation, particularly C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor alpha (TNF-α).
A 2020 systematic review examining omega-3’s effects on rheumatoid arthritis found that supplementation reduced joint pain, stiffness, and swelling. These symptoms are directly relevant to TMJ disorders. Perhaps most practically, participants were able to reduce their use of NSAIDs and avoid their side effects.
For TMJ health specifically, nutritional guidance published in dental literature emphasizes that omega-3 fatty acids are “powerful anti-inflammatory agents that can reduce swelling and discomfort in the TMJ.” Fatty fish like salmon and mackerel provide natural sources, but therapeutic doses typically require supplementation.
The evidence suggests taking at least 1 gram each of EPA and DHA daily. Research from a 2017 trial found that among people eating the least amount of fish, omega-3 supplementation was associated with a 40% reduction in heart attacks. This suggests powerful systemic anti-inflammatory effects that would benefit inflamed joints as well.
Curcumin: Nature’s COX-2 Inhibitor
If omega-3s interrupt inflammatory signaling, curcumin acts more like a pharmaceutical anti-inflammatory. Curcumin is the active compound in turmeric, but it works without the gastric side effects. Studies reviewed in Arthritis Research & Therapy demonstrate that curcumin blocks the same inflammation-promoting enzyme (COX-2) as the drug celecoxib.
In a study of 367 people with knee osteoarthritis, 1,500 mg daily of curcumin extract proved as effective as 1,200 mg of ibuprofen, without causing gastrointestinal distress. For rheumatoid arthritis, a 2023 meta-analysis examining 539 RA patients found that curcumin supplements helped reduce inflammation and symptoms, though researchers called for larger trials.
The challenge with curcumin is absorption. Standard turmeric powder contains only about 3% curcumin, and that curcumin is poorly absorbed from the gut. Modern formulations address this through several strategies: combining with black pepper extract (piperine) to boost absorption, binding to lipids, or using specialized delivery systems like liposomal or phytosomal preparations.
For TMJ arthritis specifically, clinical recommendations suggest taking curcumin with a source of fat. Some supplements include it in an oil base, or you can choose formulations enhanced with piperine. Doses studied range from 500-1,500 mg daily of standardized curcumin extract containing 95% curcuminoids.
The Synergistic Approach
What’s particularly exciting is evidence that these compounds may work synergistically. Research published in Arthritis Research & Therapy examined the combined effects of bioavailable curcumin with a vitamin D3 and omega-3 enriched diet in a collagen-induced arthritis model. The combination not only delayed disease onset but modified disease outcomes. It reduced cellular infiltration and cartilage degradation in joints.
The study’s authors note that this combination addresses multiple pathogenic mechanisms. Curcumin inhibits pro-inflammatory cytokines and NF-κB activation. Omega-3s promote specialized pro-resolving mediators that actively resolve inflammation. Vitamin D3 modulates immune function and reduces autoimmune tissue attack.
For someone dealing with nighttime bruxism causing temporomandibular joint arthritis, this suggests a rational supplementation strategy:
- Magnesium glycinate (200-400mg nightly) to reduce grinding frequency and muscle tension
- Omega-3s with at least 1g each EPA and DHA daily to suppress inflammatory cytokines
- Bioavailable curcumin (500-1,500mg daily) to inhibit COX-2 and protect cartilage
- Vitamin D3 (if deficient) to support immune regulation
For comprehensive joint support, collagen supplementation might also be considered. Research has identified specific peptide sequences from marine sources that communicate with cartilage cells to promote repair.
Beyond Supplements: The Comprehensive Approach
While nutritional interventions show promise, they work best as part of a comprehensive management strategy. Let’s be clear: supplements are not magic bullets, and they work most effectively when combined with other evidence-based approaches.
Occlusal splints remain the gold standard for protecting teeth and joints from grinding forces. Research reviewed in Physiopedia confirms that night guards reduce TMJ compression and may reduce masseter and temporalis muscle activity levels along with associated pain. These devices don’t stop the grinding behavior, but they distribute forces more evenly and create a protective barrier.
Stress management addresses root causes. Research shows 49% of US adults now report frequent feelings of stress—up from 33% in 2003. Stressed individuals show a 97% higher chance of presenting with bruxism, making psychological interventions essential rather than optional. Cognitive behavioral therapy, meditation, and biofeedback all show varying degrees of efficacy.
Physical therapy for the temporomandibular region helps maintain joint mobility and reduces muscle tension. This becomes especially important once TMJ degeneration has begun, as gentle exercises can slow progression while improving function.
Sleep hygiene optimization creates conditions for better-quality rest, potentially reducing bruxism episodes. This includes consistent sleep schedules, limiting caffeine and alcohol (both bruxism triggers), and addressing underlying sleep disorders like apnea.
Botulinum toxin injections represent an emerging option for severe cases. By temporarily paralyzing the masseter muscles, Botox reduces the force generated during grinding episodes. While not addressing the underlying behavior, it can provide several months of relief and may prevent further joint damage during that window.
The Stress Epidemic and Your Jaw
There’s a broader context worth acknowledging here. The surge in bruxism cases isn’t happening in a vacuum. According to the American Dental Association, 70% of dentists noticed increased signs of teeth grinding and clenching in their patients in 2021. This represented a 10% jump from the previous year.
What’s driving this trend? The same forces reshaping modern life: chronic work stress, social media-induced anxiety, financial pressures, political polarization, pandemic aftermath. A 2024 Gallup poll found Americans are sleeping less and feeling more stressed than ever before. November has even been designated National TMJ Awareness Month, reflecting growing recognition of these disorders’ impact.
When we discuss nighttime bruxism causing temporomandibular joint arthritis, we’re really talking about how societal stress literally grinds away at our physical structures. The jaw becomes a barometer for our collective anxiety.
This underscores why pharmaceutical or supplement-only approaches fall short. Yes, magnesium can help relax muscles. Yes, omega-3s can reduce inflammation. But if the underlying stress remains unaddressed, we’re merely managing symptoms while the root cause persists.
When to Seek Professional Help
Given the progressive nature of TMJ arthritis, early intervention matters enormously. If you’re experiencing any of the following, consult a healthcare provider:
- Morning jaw pain or stiffness that persists for more than a few weeks
- Clicking, popping, or grating sounds when opening or closing your mouth
- Difficulty opening your mouth fully
- Frequent headaches, especially upon waking
- Visible tooth wear, chipping, or fracturing
- A partner notifying you of grinding sounds during sleep
- Facial pain that radiates to the ears or temples
- Jaw that locks in the open or closed position
According to Johns Hopkins Medicine, TMJ disorders can manifest in several ways. These include myofascial pain (the most common form), internal derangement of the joint (displaced disc), or degenerative joint disease (osteoarthritis or rheumatoid arthritis in the jaw joint). You may have one or more of these conditions simultaneously.
Diagnostic evaluation typically includes a physical examination assessing jaw movement and alignment. Imaging studies (X-rays, CT, or MRI) help visualize joint structures and cartilage loss. Sometimes polysomnography is used if sleep apnea is suspected as a contributing factor.
Looking Forward: Prevention and Hope
Here’s the encouraging news: while nighttime bruxism causing temporomandibular joint arthritis represents a serious pathway to chronic pain, it’s also largely preventable and manageable when addressed early.
The research landscape continues evolving. Dr. Frank Lobbezoo at the Academic Centre for Dentistry Amsterdam has published extensively on bruxism assessment and management. His contributions to the international consensus definitions now guide clinical practice. His work emphasizes distinguishing between sleep and awake bruxism, as they may have different etiologies and require tailored interventions.
Studies from researchers like Maria Commisso at the University of Seville continue refining our understanding of the biomechanical forces at play. They use sophisticated computer modeling to predict tissue damage thresholds. This knowledge informs better protective device design and helps identify at-risk individuals before permanent damage occurs.
On the nutritional front, the convergence of evidence around magnesium, omega-3s, and curcumin offers practical tools for both prevention and management. While these supplements won’t reverse advanced arthritis, they may slow progression and reduce symptoms. This buys time for other interventions to work.
Perhaps most importantly, growing awareness means more people are taking bruxism seriously rather than dismissing it as a harmless habit. The designation of National TMJ Awareness Month in November reflects this shift. When patients and providers recognize the connection between stress, grinding, inflammation, and joint degeneration, they’re more likely to intervene before irreversible damage occurs.
Your Next Steps
If you’re grinding your teeth at night, don’t wait for jaw pain to become unbearable. The cartilage degradation process may already be underway, operating silently beneath the surface.
Consider starting with these evidence-based approaches:
- Schedule a dental evaluation to assess for signs of bruxism and TMJ dysfunction
- Optimize magnesium intake through both diet (leafy greens, nuts, whole grains, fish) and potentially supplementation with glycinate or citrate forms
- Increase anti-inflammatory foods, particularly fatty fish rich in omega-3s, or consider high-quality fish oil supplements providing at least 1g each of EPA and DHA
- Evaluate stress management strategies that resonate with you—whether meditation, therapy, exercise, or other approaches
- Consider a custom night guard if bruxism is confirmed, to protect both teeth and joints
- Address sleep quality through consistent routines and evaluation for underlying sleep disorders
Remember, your jaw joints perform thousands of movements daily. They deserve the same attention and care we give other hardworking joints in our bodies. The path from nighttime bruxism to temporomandibular joint arthritis isn’t inevitable. However, prevention requires awareness, early action, and a comprehensive approach that addresses both mechanical protection and the inflammatory processes threatening your joint health.
Have you noticed signs of nighttime grinding? What strategies have you found helpful in protecting your jaw health? Share your experiences in the comments below. Your insights might help someone else prevent permanent joint damage.
FAQ: Understanding Nighttime Bruxism and TMJ Arthritis
Q: What exactly is nighttime bruxism?
A: Nighttime bruxism, also called sleep bruxism, is a repetitive jaw muscle activity characterized by clenching or grinding of the teeth during sleep. It’s considered a sleep-related movement disorder. Unlike conscious habits, people with sleep bruxism are unaware they’re grinding and can’t control the behavior while asleep. During episodes, grinding forces can reach 250 pounds. This far exceeds the 20-40 pounds of normal chewing forces.
Q: How does bruxism cause TMJ arthritis specifically?
A: The pathway from bruxism to TMJ arthritis involves both mechanical and biochemical processes. Mechanically, excessive grinding forces create shear stresses in the temporomandibular joint’s articular disc that exceed its tensile strength. This causes microtrauma. The damage triggers release of pro-inflammatory cytokines (TNF-α, IL-1β) which stimulate matrix metalloproteinases (MMPs). These are enzymes that break down cartilage. Over time, the cartilage thins and bone begins direct contact with bone. Osteoarthritis develops. This is distinct from other TMJ problems like disc displacement or myofascial pain.
Q: What are matrix metalloproteinases and why do they matter?
A: Matrix metalloproteinases (MMPs) are a family of enzymes that break down the extracellular matrix. This is the structural scaffolding of tissues including cartilage. In healthy joints, MMPs are tightly regulated to allow normal tissue remodeling. However, inflammatory cytokines released during bruxism-related joint stress cause MMP overproduction. These enzymes degrade collagen and proteoglycans in cartilage faster than the body can repair them. This leads to progressive joint deterioration and arthritis.
Q: What are cytokines and how do they relate to TMJ inflammation?
A: Cytokines are small proteins that cells use to communicate with each other, particularly in immune and inflammatory responses. Pro-inflammatory cytokines like tumor necrosis factor-alpha (TNF-α) and interleukin-1 beta (IL-1β) signal the body that tissue is damaged. This triggers inflammation. While acute inflammation aids healing, chronic release of these cytokines perpetuates joint damage. This occurs with repetitive bruxism trauma. The cytokines stimulate enzyme production, increase oxidative stress, and promote bone resorption.
Q: What does “odds ratio of 2.25” mean in the context of bruxism and TMD?
A: An odds ratio (OR) is a statistical measure of association between an exposure and an outcome. An OR of 2.25 means people with bruxism have 2.25 times higher odds of developing temporomandibular disorders compared to people without bruxism. The confidence interval (95% CI 1.94-2.56) indicates we can be 95% confident the true odds ratio falls within this range. This confirms the finding isn’t due to chance. In practical terms: if your baseline risk of TMD is 10%, bruxism elevates it to approximately 22.5%.
Q: Why is magnesium deficiency linked to bruxism?
A: Magnesium acts as a natural calcium channel blocker and muscle relaxant. It regulates neuromuscular transmission—how nerves signal muscles to contract. When magnesium levels drop, calcium floods into muscle cells more easily. This causes increased excitability and involuntary contractions. In jaw muscles specifically, this manifests as clenching and grinding. Additionally, magnesium deficiency reduces GABA (a calming neurotransmitter) while increasing cortisol (stress hormone). This creates a neurochemical environment that promotes bruxism behaviors.
Q: What is magnesium glycinate and why is it recommended over other forms?
A: Magnesium glycinate is magnesium bound to two glycine molecules (an amino acid). This chelated form offers several advantages: (1) High bioavailability—the glycine binding protects magnesium through the digestive tract, allowing better absorption; (2) Gentle on the stomach—doesn’t cause the laxative effects common with magnesium citrate or oxide; (3) Enhanced calming effects—glycine itself has relaxing properties and may improve sleep quality. For bruxism, these characteristics make it ideal for evening supplementation at 200-400mg doses.
Q: What are EPA and DHA?
A: EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) are two primary omega-3 fatty acids found in fish oil. They’re called “long-chain” omega-3s to distinguish them from ALA (alpha-linolenic acid) found in plants. EPA and DHA have potent anti-inflammatory properties because the body converts them into specialized pro-resolving mediators—compounds that actively shut down inflammatory processes. For joint health, they inhibit inflammatory cytokine production and disrupt the NF-κB pathway that drives cartilage breakdown.
Q: What does “bioavailable curcumin” mean?
A: Bioavailability refers to the proportion of a substance that enters circulation and can have an active effect. Standard curcumin from turmeric has extremely poor bioavailability—the body absorbs only small amounts and rapidly metabolizes it. “Bioavailable” curcumin formulations use enhancement strategies: piperine (black pepper extract) blocks metabolizing enzymes; phytosomal preparations bind curcumin to phospholipids; nanoparticle formulations reduce particle size. These techniques can increase absorption by 20-fold or more, making therapeutic doses achievable.
Q: What is the temporomandibular joint’s articular disc?
A: The articular disc is a fibrocartilage structure that sits between the condyle (rounded end of the jawbone) and the temporal bone of the skull. Unlike the hyaline cartilage covering joint surfaces in knees or hips, the TMJ disc is fibrocartilage containing both Type I and Type II collagen. It functions as a cushion, absorbing force and allowing smooth gliding movements. During bruxism, sustained clenching or grinding can displace this disc or damage it through excessive shear stress, leading to clicking sounds, pain, and ultimately arthritis if cartilage wears away completely.
Q: What is the NF-κB pathway mentioned in relation to inflammation?
A: NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells) is a protein complex that controls DNA transcription and cellular responses to stimuli, particularly stress, inflammatory cytokines, and oxidative damage. When activated, NF-κB moves into the cell nucleus and “turns on” genes for inflammatory mediators, MMPs, and other destructive substances. In TMJ arthritis, chronic bruxism keeps the NF-κB pathway activated in joint tissues, perpetuating inflammation and cartilage breakdown. Many anti-inflammatory supplements, including curcumin and omega-3s, work partly by inhibiting this pathway.
Q: Can supplements really prevent arthritis from bruxism, or just reduce symptoms?
A: The honest answer is we don’t have definitive human trials specifically examining supplement prevention of TMJ arthritis from bruxism. However, the evidence suggests supplements work on multiple levels: magnesium may reduce grinding frequency (addressing the mechanical cause); omega-3s and curcumin suppress inflammatory cytokines and MMPs (interrupting the biochemical cascade of cartilage destruction). Early intervention—before significant cartilage loss—offers the best chance of prevention. Once advanced arthritis develops with bone-on-bone contact, supplements likely reduce symptoms and slow progression but won’t regenerate destroyed cartilage. Think of it as a spectrum: prevention when started early, symptom management when started late.
Q: What’s the difference between temporomandibular disorders (TMD) and TMJ arthritis?
A: TMD is an umbrella term for all disorders affecting the temporomandibular joint and associated structures—including muscles, ligaments, and nerves. TMD encompasses three main categories: (1) myofascial pain (muscle-related), (2) internal derangement (disc displacement), and (3) degenerative joint disease (arthritis). TMJ arthritis specifically refers to the third category—inflammatory degradation of joint cartilage and bone, including osteoarthritis and rheumatoid arthritis. Someone can have multiple types of TMD simultaneously, so a person might have both myofascial pain AND arthritis, both caused by bruxism.
Q: How long does it take for bruxism to cause permanent joint damage?
A: This varies tremendously based on grinding severity, duration, frequency, individual anatomy, and genetic factors affecting cartilage resilience. The finite element modeling study found that tensile strength limits could be exceeded in as little as 50 seconds of sustained maximal clenching—but this doesn’t mean arthritis develops immediately. More realistically, consider that arthritis is a progressive disease typically developing over months to years of repeated microtrauma. Some people grind for decades with minimal joint damage, while others develop symptoms within a few years. This unpredictability underscores the importance of not waiting until pain appears—by then, cartilage damage may already be significant.
Q: I’ve been grinding my teeth for years—is it too late to protect my joints?
A: It’s never too late to implement protective strategies, though earlier intervention offers better outcomes. Even if some cartilage loss has occurred, stopping further mechanical trauma (via night guards), reducing inflammation (through supplements and diet), managing stress, and physical therapy can slow or halt progression. The TMJ has some capacity for repair and adaptation, particularly in younger individuals. However, once the condition progresses to bone-on-bone contact with severe arthritis, interventions become more about pain management and preserving remaining function. The key message: start now, regardless of how long you’ve been grinding.
Q: Should I be concerned if I only occasionally grind my teeth?
A: Occasional, short-duration grinding during periods of high stress probably poses minimal risk to most people. However, several factors increase concern: frequency (nightly vs. occasional), duration (multiple episodes per night vs. brief), intensity (loud grinding audible to partners suggests high force), and whether you’re experiencing symptoms (morning jaw pain, headaches, tooth wear). Additionally, if “occasional” grinding is actually happening nightly but you’re unaware because you live alone, the risk increases. If you’re unsure about severity, consult a dentist who can examine teeth for wear patterns indicating chronic bruxism that warrants intervention.
Q: What dosages of supplements are supported by research for joint health?
A: Based on the studies reviewed: Magnesium glycinate: 200-400mg daily (taken in the evening); Omega-3 fatty acids: Minimum 1 gram each of EPA and DHA (total ~2g omega-3s) daily; Curcumin: 500-1,500mg daily of standardized extract containing 95% curcuminoids, preferably a bioavailability-enhanced formulation; Vitamin D3: If deficient, supplementation guided by blood tests, often 1,000-4,000 IU daily. These represent therapeutic ranges studied for anti-inflammatory and joint-protective effects. Always consult a healthcare provider before starting supplementation, as individual needs vary and some supplements may interact with medications.
Q: Are there any side effects or contraindications for these supplements?
A: Generally, these supplements are well-tolerated, but considerations include: Magnesium: High doses can cause diarrhea; people with kidney disease should use caution as impaired kidney function reduces magnesium excretion; Omega-3s: May increase bleeding risk in people taking anticoagulants (blood thinners) or before surgery; fish oil can cause fishy aftertaste or gastrointestinal upset in some people; Curcumin: Can enhance absorption of certain medications; piperine (often included to boost absorption) may cause liver concerns at high doses; may increase bleeding risk; Vitamin D3: Excessive supplementation can cause hypercalcemia. Drug interactions are possible with all supplements—disclosure to healthcare providers is essential.
Q: Besides supplements, what else can I do to protect my TMJ from bruxism damage?
A: A comprehensive approach includes: (1) Custom occlusal splint (night guard) to distribute forces and protect teeth—the most evidence-based mechanical protection; (2) Stress management through cognitive behavioral therapy, meditation, biofeedback, or counseling; (3) Sleep hygiene optimization—consistent schedule, dark room, avoiding caffeine/alcohol before bed; (4) Physical therapy for TMJ including gentle exercises and soft tissue mobilization; (5) Addressing underlying sleep disorders like apnea if present; (6) Limiting gum chewing and avoiding hard foods during symptomatic periods; (7) Conscious relaxation of jaw muscles during the day (setting reminders to check jaw position); (8) In severe cases, Botox injections to reduce muscle force. The best results come from combining multiple strategies tailored to individual circumstances.
Q: What’s the takeaway message about nighttime bruxism and TMJ arthritis?
A: The key insight is that nighttime bruxism isn’t just a benign habit or minor annoyance—it’s a legitimate risk factor for developing painful, potentially irreversible TMJ arthritis through a well-documented pathway of mechanical overload and inflammatory cartilage destruction. However, this progression isn’t inevitable. Early recognition and a multi-faceted approach combining mechanical protection (night guards), nutritional support (magnesium, omega-3s, curcumin), stress management, and professional care can significantly reduce risk and preserve long-term jaw function. Don’t dismiss teeth grinding as “just stress”—view it as your body’s warning signal that intervention is needed to protect one of your body’s most frequently used joints.

