Sleepwalking Amnesia and Its Relationship to Sleep Disorders: When Memory Vanishes in the Night
Story-at-a-Glance
- Sleepwalking amnesia occurs because memories are not properly formed during deep NREM sleep episodes, not simply forgotten afterward
- Partial memory retention is increasingly documented, with up to 71% of sleepwalkers reporting some dream-like recollections contrary to traditional complete amnesia beliefs
- Research challenges exist in studying sleepwalking amnesia due to inherent recall bias, making clinical assessment and treatment planning complex
- Sleep disorders connections show sleepwalking frequently co-occurs with sleep apnea, restless leg syndrome, and other disrupted sleep conditions
- Neurological mechanisms reveal that sleepwalking represents a mixed brain state where consciousness partially awakens while deep sleep persists
- Clinical implications demonstrate that effective treatment requires addressing both the underlying sleep disorder and associated memory impairments
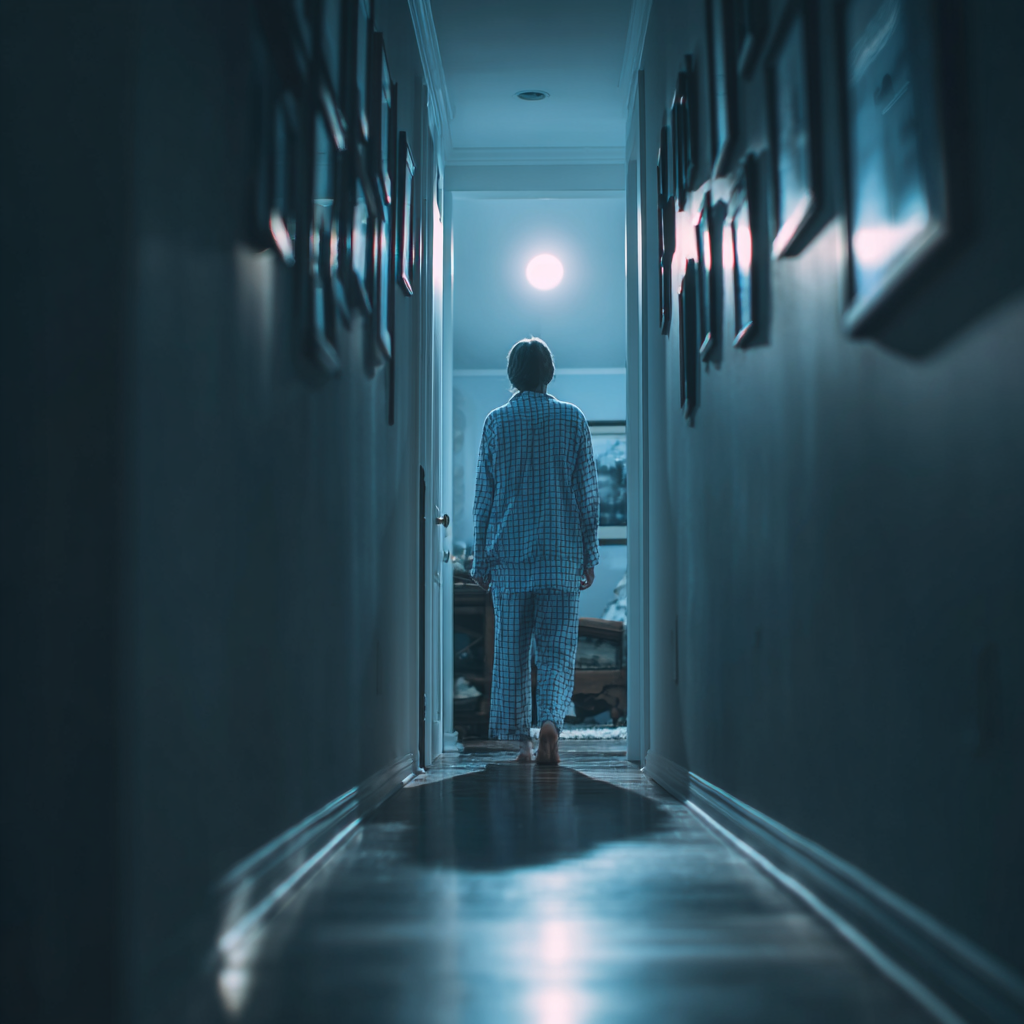
When Sarah’s husband found her in the kitchen at 3 AM methodically making a sandwich—eyes open but expression blank—she had no recollection of the event the next morning. This experience, shared by millions who struggle with sleepwalking amnesia, reveals one of sleep medicine’s most intriguing puzzles: how can someone perform complex actions yet retain no memory of them?
Sleepwalking amnesia and its relationship to sleep disorders represents far more than simple forgetfulness. According to Dr. Mark Pressman’s research, published in the journal SLEEP, “The amnesia of sleepwalking has been hypothesized to occur as a result of general higher cognitive dysfunction—memories are not formed as opposed to forgotten.”
This distinction fundamentally changes how we understand nocturnal memory loss. Rather than experiencing normal memory formation followed by forgetting, sleepwalkers exist in a unique neurological state where the brain’s memory-encoding systems remain largely offline even as motor functions activate.
The Neurological Mystery of Mixed Consciousness
The phenomenon occurs during what researchers call a “mixed brain state”—portions of the brain behaving as if awake while others remain in deep sleep. Cleveland Clinic specialists explain that during sleepwalking episodes, “parts of your brain are still asleep while others behave as if you’re awake.”
Dr. Antonio Zadra, a world-renowned expert in parasomnia research at the Université de Montréal, has spent decades investigating this complex relationship. His groundbreaking work reveals that sleepwalking amnesia and its relationship to sleep disorders involves sophisticated interactions between arousal systems and memory consolidation processes.
Recent neuroimaging studies from Zadra’s research team demonstrate altered brain perfusion patterns during both wakefulness and sleep in chronic sleepwalkers. These findings suggest that memory dysfunction extends beyond individual episodes, potentially affecting daytime cognitive function as well.
Challenging Traditional Amnesia Assumptions
The longstanding belief in complete sleepwalking amnesia is being reconsidered. Research published in multiple studies now shows that “71% of patients with a diagnosis of sleepwalking and/or sleep terrors reported at least one episode of dream-like mentation.”
This emerging evidence indicates that sleepwalking amnesia exists on a spectrum, ranging from complete memory absence to partial recollections. Some individuals retain fragmented images, emotional impressions, or narrative elements from their nocturnal episodes. Others describe dream-like sequences that may correspond to their sleepwalking behaviors.
Consider a documented case from clinical literature: researchers interviewed sleepwalking patients about “what was going through your mind at the very moment of the episodes.” Despite the inherent challenges of this type of inquiry, many patients could provide some form of response, indicating that partial memory retention occurs more frequently than previously recognized. This partial memory retention, while incomplete, provided crucial insights for understanding the spectrum of sleepwalking amnesia.
The Complex Web of Sleep Disorder Connections
Sleepwalking amnesia and its relationship to sleep disorders becomes particularly intricate when considering comorbid conditions. Mayo Clinic research identifies several underlying conditions that can trigger sleepwalking episodes:
- Sleep-disordered breathing, including obstructive sleep apnea
- Restless legs syndrome
- Gastroesophageal reflux disease (GERD)
- Circadian rhythm disruptions
Each of these conditions can fragment sleep architecture, creating the partial arousal states that predispose individuals to sleepwalking. Additionally, the sleep disruption from these disorders may compound memory formation difficulties, creating a cycle where poor sleep quality worsens both sleepwalking frequency and associated amnesia.
Dr. Yves Dauvilliers, whose landmark study examined 100 adult sleepwalkers, found that “22.8 percent of sleepwalkers presented with nightly episodes and 43.5 percent presented with weekly episodes.” His research revealed higher frequencies of daytime sleepiness, fatigue, and mood symptoms—suggesting that sleepwalking amnesia reflects broader sleep-related cognitive impairments.
Forensic and Clinical Implications
The memory challenges inherent in sleepwalking create significant clinical and legal complications. Forensic sleep medicine research demonstrates how sleepwalking amnesia complicates legal proceedings, particularly when alleged criminal behavior occurs during episodes.
The case study detailed in this research involved a defendant charged with sexual assault who claimed sleepwalking amnesia. Sophisticated polysomnography and spectral analysis revealed characteristic sleep abnormalities consistent with genuine sleepwalking disorder, ultimately supporting the defendant’s claims of amnesia.
This intersection of law and sleep medicine highlights why understanding sleepwalking amnesia and its relationship to sleep disorders requires nuanced clinical assessment. Sleep specialists must differentiate genuine parasomnia-related amnesia from other conditions that can produce similar memory gaps, including:
- Alcohol-induced blackouts
- Medication-related amnesia
- Dissociative disorders
- Temporal lobe epilepsy
Treatment Challenges and Breakthroughs
Addressing sleepwalking amnesia requires treating the underlying sleep disorder while managing safety concerns. Successful case studies from clinical literature demonstrate how psychological interventions can reduce both episode frequency and severity.
One particularly compelling case involved a 28-year-old man whose violent sleepwalking episodes ceased after addressing underlying stress and implementing sleep hygiene improvements. The psychological evaluation revealed narcissistic and aggressive tendencies that, when addressed through therapy, significantly reduced his parasomnia symptoms.
Hypnotherapy has shown remarkable success in many cases. Controlled studies demonstrate that specialized hypnotherapy sessions can provide lasting improvement in both subjective symptoms and objective measures. Follow-up evaluations at one year revealed sustained benefits, suggesting that addressing the psychological components of sleepwalking can improve associated memory dysfunction.
Additionally, many patients benefit from addressing comorbid sleep disorders. When sleep apnea treatment eliminates the fragmented sleep that triggers sleepwalking episodes, amnesia symptoms often improve dramatically.
The Stress-Memory Connection
Recent research highlights how psychological stress exacerbates both sleepwalking frequency and associated amnesia. TIME magazine’s coverage of trauma’s effects on sleepwalking reveals that “patients with PTSD have more and longer awakenings than healthy people do—they simply cannot sustain their sleep.”
This connection between emotional trauma and sleepwalking amnesia suggests that treating the psychological components may be as important as addressing the physical sleep disorder. The amygdala, which processes fear and emotional memories, shows heightened activity in trauma survivors and may contribute to the fragmented consciousness characteristic of sleepwalking episodes.
Current Research Frontiers
Dr. Zadra’s ongoing research has yielded surprising findings about the autonomic nervous system during sleepwalking. Contrary to expectations, sleepwalkers show reduced “fight or flight” responses during deep sleep, suggesting that their nervous system regulation differs fundamentally from normal sleepers.
These discoveries may eventually lead to pharmacological interventions targeting autonomic function. “Since several pharmaceutical agents can be used to modulate autonomic effects, such treatment venues could be explored if our results are replicated,” notes Zadra’s research team.
Practical Management Strategies
For individuals dealing with sleepwalking amnesia, several evidence-based strategies can help:
Sleep Hygiene Optimization:
- Maintain consistent sleep schedules
- Eliminate alcohol and sedating medications when possible
- Address underlying sleep disorders like sleep apnea
- Create a safe sleeping environment
Stress Management:
- Practice relaxation techniques before bedtime
- Address underlying anxiety or trauma through therapy
- Implement regular exercise routines (but not near bedtime)
Safety Precautions:
- Install locks or alarms on exterior doors
- Remove potentially dangerous objects from accessible areas
- Sleep on the ground floor when possible
- Inform household members about appropriate intervention techniques
The Road Ahead
Understanding sleepwalking amnesia and its relationship to sleep disorders continues evolving as research reveals the complex interplay between consciousness, memory, and sleep states. While complete amnesia was once considered universal in sleepwalking, we now recognize a spectrum of memory retention. Variation occurs significantly between individuals and episodes.
Therapeutic implications are promising. By addressing both the underlying sleep disorders and the psychological factors that contribute to episodes, many individuals can achieve significant symptom improvement. Success stories from clinical practice demonstrate important possibilities. With proper evaluation and treatment, people can reclaim both their sleep and their sense of security.
As our understanding deepens, the mysterious boundary between sleep and wakefulness becomes clearer. For the millions who experience sleepwalking amnesia, this research offers hope for better nights and clearer mornings ahead.
FAQ
Q: What exactly causes sleepwalking amnesia? A: Sleepwalking amnesia occurs because the brain exists in a mixed state during episodes—parts responsible for movement are partially awake while areas crucial for memory formation remain in deep sleep. Unlike normal forgetting, memories are never properly encoded in the first place, making them impossible to recall later.
Q: Do all sleepwalkers experience complete amnesia for their episodes? A: No. Recent research shows that up to 71% of sleepwalkers retain some form of memory from their episodes, ranging from vague emotional impressions to dream-like narratives. Complete amnesia, while common, is not universal as previously believed.
Q: How is sleepwalking amnesia different from alcohol-induced blackouts? A: While both conditions can produce similar memory gaps, sleepwalking amnesia occurs during a specific sleep stage when memory formation systems are naturally offline. Alcohol-induced blackouts result from chemical interference with memory processes during normal wakefulness. Additionally, sleepwalking episodes typically occur during the first few hours of sleep, while alcohol blackouts can happen anytime during intoxication.
Q: What is NREM sleep and why does it matter for sleepwalking? A: NREM stands for “Non-Rapid Eye Movement” sleep, which includes the deeper stages of sleep where sleepwalking occurs. Unlike REM (Rapid Eye Movement) sleep where most vivid dreams happen, NREM sleep is when your body recovers and memory consolidation takes place. Sleepwalking happens during the deepest NREM stage, which is why memory formation is impaired during episodes.
Q: What does “polysomnography” mean? A: Polysomnography is a comprehensive sleep study that records brain waves, eye movements, muscle activity, heart rhythm, and breathing patterns during sleep. It’s the gold standard test for diagnosing sleep disorders like sleepwalking. The test is usually done overnight in a sleep laboratory with sensors attached to your body to monitor various functions while you sleep.
Q: What are “parasomnias”? A: Parasomnias are a category of sleep disorders that involve abnormal behaviors, movements, emotions, or experiences during sleep. Sleepwalking is one type of parasomnia. Other examples include night terrors, sleep talking, and REM behavior disorder. The term literally means “alongside sleep” because these behaviors happen while you’re sleeping but seem like waking activities.
Q: What is the amygdala and how does it relate to sleepwalking? A: The amygdala is an almond-shaped structure deep in your brain that processes emotions, especially fear and anxiety. In people who have experienced trauma, the amygdala often becomes overactive and can trigger the partial arousals from deep sleep that lead to sleepwalking episodes. Think of it as your brain’s alarm system that sometimes goes off at the wrong time.
Q: Can treating underlying sleep disorders help with sleepwalking amnesia? A: Yes, absolutely. Conditions like sleep apnea, restless leg syndrome, and other disorders that fragment sleep can trigger sleepwalking episodes. Successfully treating these underlying conditions often reduces both the frequency of sleepwalking and associated memory problems.
Q: What is sleep apnea? A: Sleep apnea is a condition where breathing repeatedly stops and starts during sleep, causing brief awakenings that can fragment your sleep. These interruptions can trigger sleepwalking episodes in susceptible people. It’s often characterized by loud snoring and feeling tired despite a full night’s sleep.
Q: Is sleepwalking amnesia dangerous? A: The amnesia itself isn’t dangerous, but it can create safety concerns because individuals may engage in potentially harmful activities without memory of them. This makes it crucial to create safe sleeping environments and address underlying triggers to reduce episode frequency.
Q: What is hypnotherapy and how does it help sleepwalking? A: Hypnotherapy is a form of therapy that uses guided relaxation and focused attention to help people change behaviors or responses. For sleepwalking, specialized hypnotherapy techniques can help reduce episode frequency by addressing underlying stress and teaching the mind to maintain deeper, more stable sleep. It’s different from stage hypnosis and is conducted by trained medical professionals.
Q: Can psychological therapy help with sleepwalking amnesia? A: Research demonstrates that psychological interventions, including hypnotherapy and stress management, can significantly reduce sleepwalking frequency and severity. By addressing underlying psychological factors like stress, trauma, or anxiety, many people experience improvement in both their sleepwalking episodes and associated memory issues.

